Building Better Healthcare Teams
WHAT we do
The mission of the UVA Center for Interprofessional Collaborations (CIPC) is to improve patient care and build more cohesive healthcare teams by promoting interprofessional collaborative education, research, and practice.
WHY we do it
Every person seeking healthcare deserves a cohesive and collaborative team of experts addressing their needs. Overwhelming evidence supports the notion that interprofessional collaborative practice (IPCP) improves the quality of care provided, decreases medical errors, improves outcomes, and enhances patient satisfaction. Well-functioning teams also work more efficiently, contributing to reduced healthcare costs.
Despite best intentions, many healthcare teams struggle with coordinating their efforts. Challenges such as long-standing routines, differing communication styles and tools, misunderstandings about one another's roles and workflow, and differing priorities can complicate our ability to work together.
Interprofessional education (IPE) and team training for collaborative practice address these challenges. By providing opportunities to learn with, from, and about one another, IPE and Team Training allow for the creation of shared mental models, the development of respectful relationships, and improved communication.
When teams work together well, everyone benefits.
HOW we do it
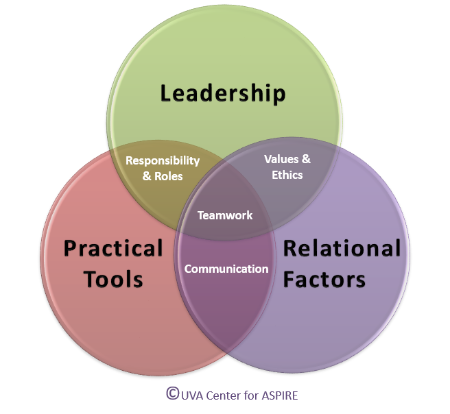
The UVA ASPIRE Model provides a framework that helps us operationalize and embed the Interprofessional Education Collaborative (IPEC) core competencies into the design of IPE and Collaborative Practice educational activities. As we created programs at our institution, we identified three primary challenges that stood out as areas where our training could help contextualize the IPEC competencies and help our learners. Those areas are PRACTICAL TOOLS, LEADERSHIP TRAINING, and information about RELATIONAL FACTORS.
PRACTICAL TOOLS are an important component of IPE, whether targeting early learners, clinician teams, or faculty educators. Resources such as ice-breakers, reflective prompts, simulation scripts, and debriefing guides provide structure and focus that engage learners and help them apply their new knowledge to clinical care. Assessment of IPE also depends on practical tools like surveys, online modules, and observational checklists. Providing these materials help our learners from having to "reinvent the wheel."
LEADERSHIP in interprofessional teams has unique nuances. Who the leader is at any given moment depends on the situation. All members of the team need to recognize what each of the other members of the team needs to succeed – because each of them is likely to lead at some point. Leadership Models can create a shared understanding of leadership built on a foundation of interpersonal decision-making, individual development, and communication.
The relationships between team members greatly influence the team's ability to function. When respectful relationships are created, the likelihood that a team will succeed is enhanced, and the opportunities for synergy are expanded dramatically. Providing IP team members with training in RELATIONAL FACTORS gives them skills to form relationships, appreciate team dynamics, create shared mental models, and anticipate and constructively deal with conflict.
Using the UVA ASPIRE Model has helped us design, implement, assess, and evaluate our IP activities across the learning continuum. It anchors the IPEC Competencies in a foundation that intuitively makes sense to our learners and addresses the challenges that they are experiencing. For more information about this unique framework:
- Read the 2019 UVA ASPIRE Model article featured in the Journal of Interprofessional Care
- Watch the short video (below) about the development and use of this unique approach to framing the core IPEC Competencies